What is Trigeminal Neuralgia?
Trigeminal neuralgia (also known as tic douloureux) describes a condition that affects the trigeminal nerve. Also known as the fifth cranial nerve, its role is to help certain areas of the face to move and detect sensations. As the largest of the 12 cranial nerves, it is responsible for innervating areas around the forehead, cheeks, nose and jaw. Any injury to this nerve can lead to symptoms and problems in these areas.
According to the Trigeminal Neuralgia Association Australia [1], approximately 25000-50000 Australians live with trigeminal neuralgia. Women and those over 50 are more likely to be diagnosed with this condition [2].
Trigeminal nerve pain around the eyes, lips, cheeks, nose and jaw is the most commonly reported symptom. For many, these symptoms only appear for specific periods ranging from days to months before recurring sometime in the future.
 
Trigeminal Neuralgia Symptoms
Symptoms of trigeminal neuralgia are often present on one side of the face and certain parts along the cranial nerve. As the trigeminal nerve is split into three branches (known as the mandibular, maxillary and ophthalmic nerves), symptoms can occur either in a single or a combination of these zones (as seen in the image below). More commonly, symptoms will be experienced along the mandibular and/or maxillary regions.
 
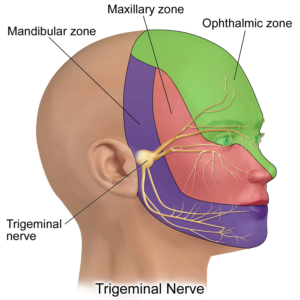
 
Sourced from: https://commons.wikimedia.org/wiki/File:Trigeminal_Nerve.png
 
 
Patients often describe their symptoms as [1][2]:
- Sharp pain on the side of the face (people can describe this as feeling like a ‘lightning bolt’)
- Facial nerve pain
- Facial numbness
- Symptoms that come and go
- Muscle spasms along the face
- Burning and tingling sensations
- Increased sensitivity
- Facial twitches
 
Trigeminal Neuralgia Causes
Causes of trigeminal neuralgia can vary from person to person. However, the most common underlying root cause of this condition is due to abnormal activity along the trigeminal nerve. The breakdown of coating (called the myelin sheath) around part(s) of the nerve causes the unusual firing of the nerves to the face. This process is also known as ‘demyelination’.
Researchers have suggested three potential diagnoses of trigeminal neuralgia, which explains how this demyelination occurs [2][3]:
- Classic trigeminal neuralgia: Compression to the surrounding nerves or blood vessels surrounding part(s) of the trigeminal nerve. The superior cerebellar artery (which is located around the brainstem) is potentially one of the most common compressed area
- Secondary trigeminal neuralgia: Other conditions may also impact the trigeminal nerve, including multiple sclerosis, abnormal arteries and tumours.
- Idiopathic trigeminal neuralgia: Unknown reasons.
 
Trigeminal Neuralgia Triggers
Despite the changes to the trigeminal nerve, symptoms occur in waves, usually lasting only seconds [1]. These episodes occur throughout the day and can last anywhere between days to months. Eventually, these symptoms disappear and appear (for days to years at a time). However, there can be triggers that can lead to these symptoms from reappearing, including:
- Being touched (e.g. pinching the cheeks, shaving, brushing teeth, etc.)
- Certain movements (e.g. eating, speaking, singing, eating, etc.)
- Hot and/or cold temperatures
- Certain surgical procedures
- Stress
 
Is Trigeminal Neuralgia Contagious?
Most cases of trigeminal neuralgia are not contagious. However, certain transmissible viruses, such as the herpes virus, can also lead to trigeminal neuralgia [4].
 
Tests and Diagnosis
Your GP can make a diagnosis based on the description of your symptoms, including the location of pain, type of discomfort, triggers and your medical history. Additionally, a physical and/or neurological examination may also be performed. However, your GP may also request further testing to confirm the diagnosis.
Imaging
Although not always necessary, MRI imaging (click here for more information) can be performed to look for certain conditions (e.g. tumours, blood vessel abnormalities, etc.) which could be causing trigeminal neuralgia [5].
 
Trigeminal Neuralgia Treatment
Treatment for trigeminal neuralgia can vary depending on the duration, severity and success of previous options. Examples of some treatments that your GP may recommend includes:
Medication
Anticonvulsant medications, such as carbamazepine, are commonly prescribed by doctors to treat nerve pain, such as trigeminal neuralgia [5]. Your GP may also recommend other medications which may assist with your symptoms.
Surgery
Surgery may also be another option for those with persistent symptoms and/or the presence of other related conditions. A popular procedure called a microvascular decompression helps reduce the pressure from the compressed blood vessel(s). Although there is a 90-95% success rate, symptoms have been reported to eventually recur [5].
Medical Specialist
Referrals to medical specialists, such as neurologists, might be recommended by your GP. Neurologists are specially trained doctors who look after conditions of the brain, spinal cord, nerves and muscles. Their specialised skill sets allow for comprehensive diagnosis, prescribing alternative medications and advanced treatment options.
 
Complications
While not a life-threatening condition, trigeminal neuralgia can severely impact the quality of life. Patients may be reluctant to perform specific actions that could trigger their symptoms, such as eating certain foods and speaking. This can impact participation in social events and activities. Compounding limitations from trigeminal neuralgia may even lead to self-confidence, anxiety and mental health issues.
Other complications can include [2]:
- Ongoing symptoms on the affected side(s) of the face
- Weakness along the jaw muscles
- Side effects from taking the medication or undergoing surgery
 
Recovery
Typically, symptoms of trigeminal neuralgia will appear over days to months. This is followed by intervals of symptom-free periods. However, symptoms can often return and sometimes even worsen over time [2].
However, research has suggested that those who receive proper medical treatment have favourable outcomes [6]. When receiving a combination of medical, physiotherapy, psychological and/or surgical treatment, half of those with trigeminal neuralgia saw a 50% improvement of symptoms.
Always seek the assistance of your GP for comprehensive treatment and to optimise your recovery.
 
 
Receiving quality care from highly experienced doctors is essential for a prompt diagnosis and receiving the correct medical treatment. With 24-7 MedCare, you can experience telemedicine from the convenience of your own home. Our friendly online doctors will be available 24/7 for a consultation, anytime and anywhere in Australia.
To make a telehealth appointment booking, simply click on the button below.
 
 
 
 
References
- https://tnaaustralia.org.au/what-is-tn/
- Shankar Kikkeri N, Nagalli S. Trigeminal Neuralgia. [Updated 2021 Nov 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554486/
- Gambeta, E., Chichorro, J. G., & Zamponi, G. W. (2020). Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Molecular pain, 16, 1744806920901890. https://doi.org/10.1177/1744806920901890
- https://hhv-6foundation.org/bells-palsy/hhv-6-is-the-most-common-virus-found-in-trigeminal-and-facial-nerves
- Quail, G. (2005). Atypical facial pain: a diagnostic challenge. Australian family physician, 34(8).
- Heinskou, T.B., Maarbjerg, S., Wolfram, F. et al. Favourable prognosis of trigeminal neuralgia when enrolled in a multidisciplinary management program – a two-year prospective real-life study. J Headache Pain 20, 23 (2019). https://doi.org/10.1186/s10194-019-0973-4

